Skin cancer ranks among the most common cancers worldwide. While melanoma often receives the most attention, non-melanoma skin cancer (NMSC) is actually far more prevalent, affecting millions annually. Fortunately, when detected early, most NMSC cases respond well to treatment. This guide explains what NMSC is, its warning signs, and prevention methods.
What is Non-Melanoma Skin Cancer?
Non-melanoma skin cancer refers to a group of cancers that develop in the skin but are not melanoma. The two most common types are:
- Basal Cell Carcinoma (BCC)
- Squamous Cell Carcinoma (SCC)
What Causes Non-Melanoma Skin Cancer?
The primary cause of NMSC is excessive exposure to ultraviolet (UV) radiation from the sun or artificial sources like tanning beds. Other risk factors include:
- Fair skin that burns easily
- Prolonged sun exposure or history of sunburns
- Weakened immune system
- Exposure to radiation or harmful chemicals
- Family history of skin cancer
Before discussing NMSC, it's important to address precancerous lesions, as these common conditions can often be prevented from developing into cancer with early and proper treatment.
Precancerous Lesions
These include actinic keratosis, Bowen’s disease and actinic chelitis.
Actinic keratosis
These appear as small, rough, scaly patches on areas of skin that have had a lot of sun exposure. Actinic keratosis often affects larger patches of skin, known as “field cancerization,” where both visible and hidden lesions may form. Treating these lesions is important, as they have the potential to develop into squamous cell carcinoma, a type of skin cancer.

Image 1. Actinic keratosis on the scalp
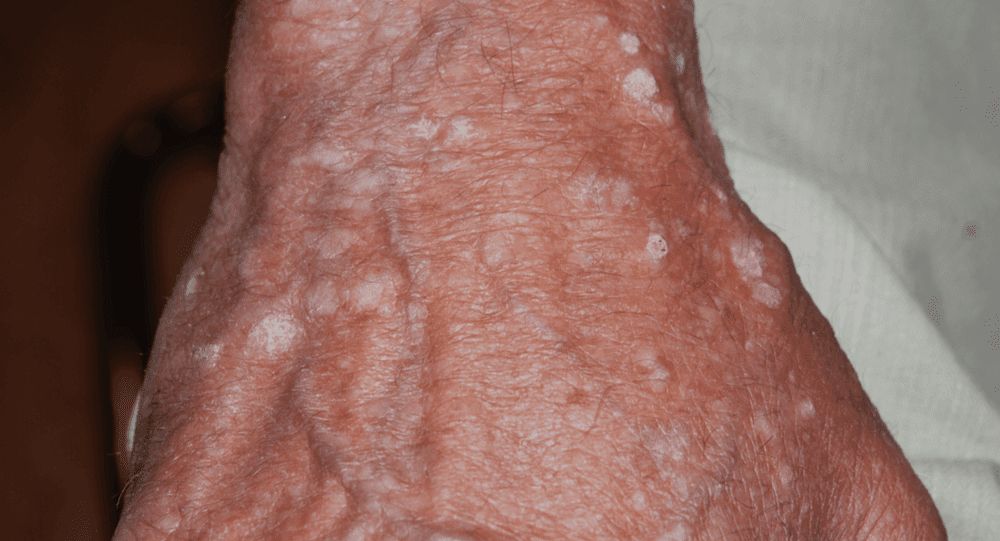
Image 2. Actinic keratosis on the back of a hand
Treatment Options for Actinic Keratosis
The best treatment for actinic keratosis depends on the severity of the condition and the individual’s health history. Here are some common approaches:
- Topical Medications: These are creams or gels that you apply directly to the affected skin, usually once or twice a day for a few weeks. Medications that are topical chemotherapy or immunotherapy work by destroying abnormal cells, allowing new, healthy skin cells to grow in their place.
- Cryotherapy: This quick treatment involves freezing the affected area with liquid nitrogen, causing the damaged cells to die and flake off. New, healthy skin cells then replace the old ones. Cryotherapy is done in a doctor’s office and is usually only mildly uncomfortable.
- Curettage and Electrodesiccation: For this procedure, the doctor scrapes off the abnormal area with a tool, then applies a low-level electric current to remove any remaining damaged cells. This procedure is typically done under local anesthesia (numbing) and can sometimes leave a small scar.
- Photodynamic Therapy (PDT): PDT combines a special light-sensitive solution with a targeted light. First, the solution is applied to the skin, where it is absorbed by the abnormal cells. Then, a light source is used to activate the solution, destroying the affected cells while allowing new skin cells to grow. This is usually done in a clinic setting and may cause mild discomfort during treatment.
- Laser Therapy: Laser therapy uses a highly focused laser beam to target and destroy abnormal cells. This treatment is often done under local anesthesia and may need to be repeated for best results. The laser allows precise targeting, helping to treat only the affected skin.
Bowen's disease
Bowen's disease appears as red, scaly patches on the skin and is also known as "squamous cell carcinoma in situ"—an early form of skin cancer that remains confined to the top layer of skin. It typically develops in sun-exposed areas and occurs more frequently in older adults and those with weakened immune systems. While its precise cause remains unclear, long-term sun exposure, chronic skin irritation, and genetic factors appear to play key roles.
Bowen’s disease can easily be mistaken for a patch of eczema, but it doesn’t respond to conventional eczema treatment. Without treatment, Bowen's disease may develop into invasive squamous cell carcinoma, which has the potential to spread throughout the body.

Image 3. Bowen’s disease
Treatment Options
Treatment choice depends on the patch's size, location, and severity, as well as the patient's overall health. For larger or isolated patches, surgery is typically recommended to remove the abnormal area completely. Smaller lesions may respond well to alternative treatments like cryotherapy, topical medications, photodynamic therapy, or laser therapy. Your dermatologist will recommend the most suitable option for your specific case.
Actinic cheilitis
This condition, sometimes called "Sailor's Lip," affects the lips and can develop into skin cancer if left untreated. Like actinic keratosis, it stems from long-term sun exposure and is considered a precancerous change in the skin. It typically appears on the lower lip, specifically along the border where the lip meets the skin.

Image 4. Actinic chelitis
Because squamous cell carcinoma (SCC) on the lips is more likely to spread than in other areas (about an 11% chance compared to 1% on other body parts), it’s especially important to recognize and treat actinic cheilitis early.
Treatment Options
Treatment for actinic cheilitis is similar to that for actinic keratosis, including options like topical creams, freezing the area (cryotherapy), laser treatment, or photodynamic therapy.
Non-Melanoma Skin Cancer (NMSC)
Non-melanoma skin cancers comprise two main types: basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). Let's explore BCC, the more common type.
Basal Cell Carcinoma (BCC)
Basal cell carcinoma (BCC) is the most common type of skin cancer, affecting millions of people annually. It is in fact the most common cancer worldwide. While it rarely spreads to other parts of the body, BCC can grow into surrounding tissues and cause significant damage without treatment. The cancer typically develops on sun-exposed areas such as the face, neck, and ears. It presents as a small, shiny bump or nodule, often with visible blood vessels on its surface. When irritated, the bump may scab.

Image 5. BCC
Treatment Options
BCC is highly treatable, and various options are available depending on the lesion's size, location, and risk level. The gold standard for treatment is surgery, particularly a technique called Mohs surgery for high-risk cases, where the cancer is removed in thin layers while minimizing damage to healthy tissue. For small, low-risk BCCs, options may include:
- Cryotherapy (freezing the cancer cells)
- Topical creams like imiquimod or 5-FU, which help destroy cancer cells
- Photodynamic therapy (PDT), which uses a special light after applying a sensitizing solution to target abnormal cells
For older patients or cases where surgery isn’t ideal, radiation therapy may also be considered.
Your healthcare provider can help you decide on the best treatment approach, balancing effectiveness with the cosmetic outcome to ensure minimal visible impact on your skin’s appearance.
Cutaneous Squamous Cell Carcinoma (SCC)
Cutaneous squamous cell carcinoma, or SCC, makes up about 20% of all skin cancers. This type of skin cancer is becoming more common, especially as the population ages.
How to Recognize SCC
SCC often appears as a rough, scaly patch, a red or pink bump with a dip in the middle, or a sore that doesn’t heal. It can sometimes resemble a wart-like growth. SCC is usually found on sun-exposed areas, like the face, hands, and neck. Unlike basal cell carcinoma (BCC), SCC has a slightly higher chance of spreading (metastasizing) to other parts of the body if it’s left untreated, which can make early detection and treatment especially important.

Image 6. SCC
Treatment Options for SCC
Most SCC cases can be treated effectively, usually with surgery. Here are some of the most common treatments:
- Surgical Excision: The tumor is removed surgically along with a small margin of surrounding healthy tissue to ensure no cancer cells remain.
- Mohs Surgery: This is a precise surgical technique often used on high-risk SCCs, especially those on the face or other sensitive areas. It allows for the removal of cancer while saving as much healthy tissue as possible.
- Cryosurgery: For smaller or lower-risk SCCs, freezing the cancer cells with liquid nitrogen can be an option.
- Electrodessication and Curettage: This involves scraping away the cancer cells and using an electric current to destroy any remaining cells. It’s often used for small or superficial SCCs.
- Radiotherapy: Radiation can be a good alternative, especially for patients who may not be candidates for surgery.
- Topical Medications and Photodynamic Therapy: These may be used for early-stage or low-risk SCCs, particularly if surgery is not feasible.
The choice of treatment depends on the size, location, and risk level of the lesion. In some cases, SCCs may recur or spread, so regular follow-up with a healthcare provider is essential to monitor for any signs of recurrence.
Prevention Tips
The best way to prevent NMSC is to protect your skin from excessive UV exposure. Here’s how:
- Wear sunscreen with at least SPF 30 every day, even on cloudy days. - Seek shade during peak sun hours (10 a.m. to 4 p.m.).
- Wear protective clothing, hats, and sunglasses.
- Avoid tanning beds and sunlamps.
- Regularly check your skin for changes and see a dermatologist for routine skin exams.
Conclusion
Non-melanoma skin cancer (NMSC) is largely preventable with proper sun protection practices starting from a young age. It’s essential for everyone to take steps to shield their skin from the sun's harmful rays. This includes wearing protective clothing, applying sunscreen with a high SPF regularly, and seeking shade during the peak hours of sun exposure.
In addition to these protective measures, it’s important for individuals to monitor their skin for any changes or unusual spots, and to consult a healthcare provider if they notice any suspicious growths or lesions. Awareness and early detection of precancerous and cancerous lesions can significantly reduce the risks associated with these conditions. By adopting these proactive strategies, people can minimize their chances of developing NMSC and maintain their overall health and well-being for years to come.

















